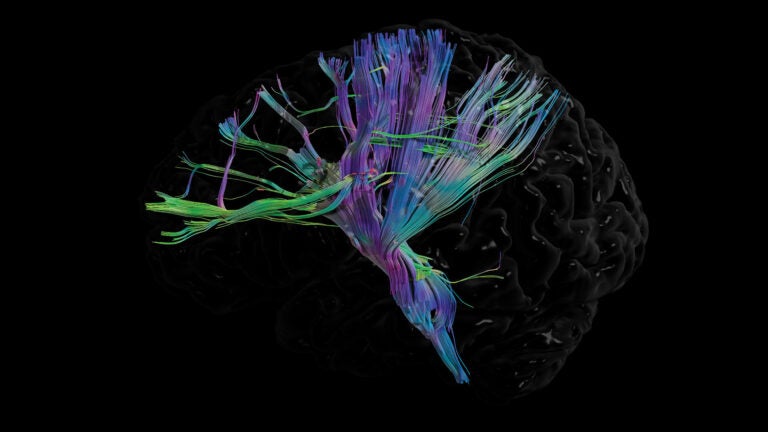
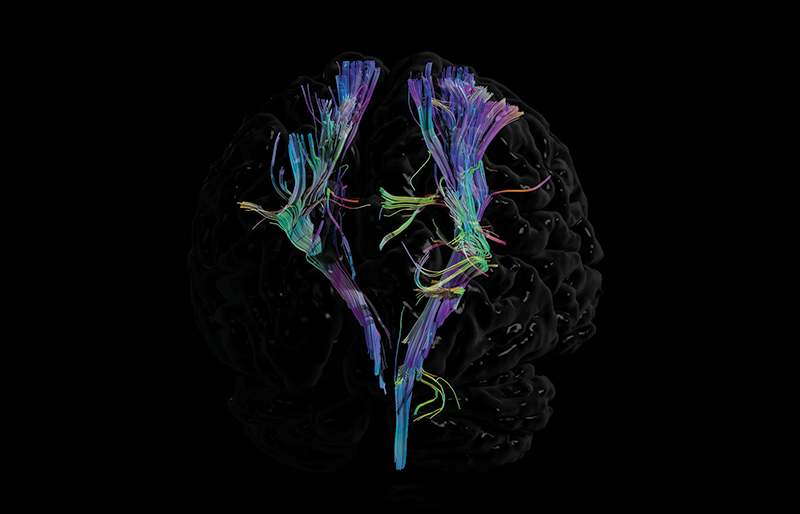
A powerful 7T MRI scanner at USC can give scientists a better look at internal structures, like the corticospinal tract of our brain. (Photo/Image courtesy of Jim Stanis, Arthur W. Toga, and the USC Mark and Mary Stevens Neuroimaging and Informatics Institute)
Tech Advances That Help Doctors Find and Treat Disease Earlier Than Ever
When disease hides in the body, it takes some big ideas from scientists and doctors to illuminate it — and save lives.
A lot has changed for Rachel Moayedi in two years.
She has lost 20 pounds. Her “chipmunk cheeks,” as she calls them, have melted away. Oh, and the 33-year-old has a baby. Her sweet little girl, Sadie, arrived last autumn.
The transformations in Moayedi’s life are thanks in large part to a cutting-edge machine that spotted a tumor in her brain. It took the powerful 7T magnetic resonance imaging (MRI) scanner at the USC Mark and Mary Stevens Neuroimaging and Informatics Institute to help radiologists pinpoint the small mass that other imaging scans hadn’t seen.
Ever-stronger scanners like the one at USC represent the latest step toward a long-standing dream for doctors and scientists alike: being able to detect early signs of disease from outside the body. In addition to MRI and other advances in medical imaging, USC physician-scientists are experimenting with technology that can spot single cancer cells in the bloodstream, sense early signs of an impending heart attack and more.
It’s all meant to keep people happy, healthy and whole. Just ask Rachel Moayedi.
7T MRI Scanner: Advances in Medical Imaging Illuminate Hidden Disease
 Despite years of infertility treatments, Moayedi couldn’t get pregnant and no one was sure why. But looking back, she says, that wasn’t the only thing wrong with her body.
Despite years of infertility treatments, Moayedi couldn’t get pregnant and no one was sure why. But looking back, she says, that wasn’t the only thing wrong with her body.
“I had these cheeks, like chipmunk cheeks, that were always red,” she says. “I had this pouch on my belly that was always soft and wouldn’t go away.” No matter how carefully she ate, she gained weight. She bruised surprisingly easily. And she always felt tired.
Then one day in 2019, her acupuncturist asked if anyone had checked her thyroid levels. So began an odyssey that had Moayedi zigzagging among doctors, laboratories and MRI scanners. She learned her thyroid levels were irregular. Her cortisol — a stress hormone — was sky high. Her own internet research led her to believe she might have Cushing’s disease. The condition can occur when a benign tumor in the pituitary gland, a pea-sized organ in the brain, causes the gland to secrete too much adrenocorticotropic hormone. That, in turn, triggers the adrenal glands to overproduce cortisol, which can lead to many of the symptoms Moayedi experienced.
But in April 2019 when she underwent an MRI scan in San Diego, where she lives, the results were inconclusive. “Tiny pituitary microadenoma cannot be excluded,” read the report. In other words, the existing imaging technology wasn’t powerful enough to see a small mass — or rule it out.
USC’s high-powered 7T MRI scanner allows scientists and doctors to peer into the human body and detect health issues much sooner than previously possible.
Her husband refused to accept that ambivalent result and began researching other options. “He said: ‘We want you to be seen by a specialist, people who see this [condition] all day, every day and know what they are doing,’” Moayedi recalls. Then he spotted a mention of USC’s 7T MRI scanner.
The “T” stands for tesla — not the car brand but rather a unit of measurement used to quantify the strength of a magnetic field. The average MRI strength is three teslas, or 3T. The 7T MRI “is a leap forward in terms of resolution,” says brain scientist Arthur W. Toga, director of the USC Stevens Neuroimaging and Informatics Institute, Provost Professor and the Ghada Irani Chair in Neuroscience. The new scanner, acquired four years ago, has allowed Toga and his colleagues to see into the living brain in ways that weren’t possible before.
For instance, one focus of Toga’s research is Alzheimer’s disease and how it changes the brain’s structure. His team looks at a part of the brain called the hippocampus — which plays a major role in learning and memory — to see how much it shrinks under the burden of the disease. With standard scanners, Toga can see the hippocampus but can’t delve into its many features. “At 7T, I can,” he says. “I can begin to tease apart what part of the hippocampus is being affected.”
Thanks to the 7T MRI scanner, Toga and his colleagues can also see changes happening in the spaces around the brain’s blood vessels as Alzheimer’s disease progresses. “Without this powerful scanner,” he says, “it’s hard to quantify what is happening.”

To scan a part of the body, the machine needs an antenna, or coil, to collect data from that area. So far, this 7T MRI scanner has a coil for the head and another for the knees.
That’s more than enough to spark the imagination of Vishal Patel, an assistant professor of radiology at the Keck School of Medicine of USC. “You immediately look at a 7T MRI scan and realize it’s something you haven’t seen before,” he says.
As a neuroradiologist, he learned about the intricacies of brain structure by studying images from scanners and consulting with pathologists, who examine tissue under the microscope. But their descriptions feel like a blurry jumble now that he has seen the quality of images from the 7T MRI scanner. “It’s fantastic to be able to see the anatomy in such great detail,” he says.
He also sees exciting progress with patients like Moayedi, who have pituitary tumors so small they can’t be detected with 3T MRI. In a study Patel published in the journal Neuroradiology in April 2020, radiologists detected a previously unseen lesion in nine of 10 patients who underwent a scan. Of those nine, Patel says, eight then underwent surgery that relieved their symptoms and changed their lives. Moayedi is among them — her tumor was removed in June 2019 by a USC team that included neurosurgeon Gabriel Zada and endocrinologist John Carmichael.
But Patel isn’t ready to stop there. He ticks off a long list of vexing brain diseases and conditions that might be treated more precisely by performing advanced medical imaging using the 7T MRI scanner: multiple sclerosis, migraines, Alzheimer’s disease and seizure disorders. These high-powered scanners, Toga adds, hold immense promise for the field of neuroimaging.
“By allowing us to visualize increasingly small regions of the brain,” he says, “it brings us one step closer to understanding structure and function at the cellular level.”
USC Experts Seek Early Signs of Cancer Before It Spreads
A malignant tumor in a breast isn’t necessarily lethal. But it could become deadly when it starts spreading.
USC experts are pioneering liquid biopsy procedures that could help doctors treat cancer before it spreads.
Technology developed at the USC Michelson Center for Convergent Bioscience aims to detect when that happens, spotting cancer cells as they move around the body hunting for places to spread and multiply. So-called liquid biopsies look for those cells in the bloodstream, spinal fluid and bone marrow — anywhere cancer might try to hitch a ride.
That’s where Peter Kuhn comes in. “There’s a very basic question: Can we diagnose cancer with a blood draw?” says Kuhn, a founding member of the USC Michelson Center and director of the center’s Convergent Science Institute in Cancer. “If we can do that, we could make life as a patient so much easier. We could make the job of our health care system so much more effective and efficient.”
It’s no simple matter for malignant cells to survive away from their source, says Kuhn, Dean’s Professor of Biological Sciences at the USC Dornsife College of Letters, Arts and Sciences.
“The cancer cell has to somehow get from that primary location, through the blood, to some other destination, settle down and start growing,” he says. “That means the cancer has to overcome so many challenges. When it manages to do that, it is a really bad cancer. It has trained up to survive.”
For nearly two decades, Kuhn has led the effort to detect early signs of the most tenacious, metastasizing cancers. In 2009, his lab launched a startup company, Epic Sciences, to license its technologies and develop clinical studies to prove their utility. That company has now received regulatory approval for a liquid biopsy test designed to detect cancerous cells that have broken away from a prostate tumor. These cells — now circulating in the bloodstream and resistant to certain drugs — are a sign that the cancer is aggressive and requires a new treatment approach. The company is testing a similar technology for breast cancer.
“The blood is the superhighway that connects the body,” Kuhn says. “I can draw blood much more easily than I can do a biopsy by sticking a long needle through my rib cage to an organ.”
If doctors can spot these metastasizing cancer cells before they grow and show up as a tumor on a scan, they could potentially deliver chemotherapy sooner and give patients a better chance of recovering from the disease.
A Colorful Solution to Detect Early Signs of Cancer
 A love of Disney animation led engineer Cristina Zavaleta to rethink the tools physicians use to pinpoint tumors.
A love of Disney animation led engineer Cristina Zavaleta to rethink the tools physicians use to pinpoint tumors.
One of her hobbies is art, and she indulged herself by signing up for a workshop in Emeryville, California, led by Pixar animators. “I was exposed to all these different paints, and they were vibrant colors,” says Zavaleta, assistant professor of biomedical engineering at the USC Michelson Center. “At the same time, I was working on my research and thinking about imaging and new contrast agents. I started thinking about what pigments are being used in humans already.”
Tattoo inks came to mind. So did snacks and drinks with food coloring. Drugs contain dyes. Cosmetics like lipstick and eyeliner come in every shade imaginable. She wondered: Could any of these dyes also be injected or ingested for a medical procedure? And if so, what could they illuminate that current contrast agents cannot?
So began her quest to help diagnose and treat cancer by bringing together common household dyes with tiny specks of matter — what scientists call nanoparticles. (To understand how small a nanoparticle is, Zavaleta says, picture a chocolate-covered donut about 4 inches across. Now imagine it with little round rainbow sprinkles. In terms of size, a donut is to a sprinkle as a cell is to a nanoparticle.)
A new nanoparticle developed by USC researchers could treat atherosclerosis — a dangerous condition linked to heart attack and stroke.
Here’s how cancer detection often works today: A physician suspects a patient has cancer in part of her body but wants to know more before recommending treatment or surgery. That patient receives an injection (or swallows a liquid) that contains a contrast agent, or dye. If a tumor exists, it can be illuminated by the agent so that it shows up on an imaging scan.
Zavaleta wants to make the dyes even more powerful so that tumors show up even clearer than they do now. When scientists chemically hook the dyes up to nanoparticles, the resulting contrast agent could make its way into a tumor and light it up brighter and for longer than current contrast agents.
The agents could also illuminate other conditions in the body, like plaque on artery walls or inflammation triggered by arthritis. The nanoparticle-encapsulated dyes, Zavaleta explains, “can be targeted to anything you want to glow for you.”
At the moment, her dye technology exists only in the lab. Human trials are years off, pending federal approval. But Zavaleta and her fellow scientists already believe that dye-infused nanoparticles have the potential to spotlight cancer more accurately.
Technology That Could Stop Heart Attacks Before They Start
The hallmark of high cholesterol is the fat deposits it coats along your artery walls, forming plaque. When a chunk of this plaque buildup ruptures, it can trigger bleeding and blood clots. One of those clots could lodge in a spot that blocks a key artery, causing a heart attack or stroke.
But what if doctors could spot the bits of plaque in your body that might be about to break open and stabilize them with a protective coating? USC doctoral student Deborah Chin has come up with nanoparticles that could help them do just that.
Chin’s idea is to find potentially dangerous plaque on artery walls — what’s called atherosclerosis. Physicians today focus on slowing down the progress of atherosclerosis to prevent heart attack and stroke. They do that by cutting levels of the dangerous form of cholesterol in the blood. Patients often take statin drugs to reduce high cholesterol levels. But sometimes those drugs aren’t enough to prevent plaque from building up and rupturing.
The nanoparticle Chin developed could identify any existing plaque that is inflamed and poses a danger. It would carry materials that bind the nanoparticle to the inflamed area, strengthening the damaged tissue. And because a contrast agent can also be paired with the particle, the worrisome plaque could show up on an MRI scan.
So far, Chin says method has worked successfully with animal models. Human trials remain about 10 years away for her technology, but science will steadily march on. Other lifesaving methods that detect early signs of disease that were once major advances, like mammography and colon cancer screening tools, are now commonplace. Imaging technology is constantly improving.
Rachel Moayedi can vouch for that.
The 7T MRI technology that enabled USC doctors to see the mass on her pituitary gland was unheard of only a decade ago — and even more powerful MRI scanners are in development. Six months after Moayedi benefited from the 7T MRI scanner at the USC Stevens Neuroimaging and Informatics Institute, she was feeling better, looking better and best of all, pregnant with her daughter.
“The 7T MRI was a game changer for our family,” Moayedi says. “We owe the researchers, Dr. Zada and Dr. Carmichael my life.”



