USC Researchers Race to Get Ahead of Alzheimer’s
More than 70 USC researchers, physicians and scientists work to unlock the mysterious disease.
Ron Kooper had been an art teacher in San Pedro, California, for three decades, patiently guiding hundreds of students through drawing, sculpting and painting. But the year before he had planned to retire, he told his wife, Eleanor, that he wanted to leave his profession and move to the desert. “It was very unlike him,” Eleanor Kooper recalls. They made the move, and even set up a tiny art studio behind their house in La Quinta—but he never again painted or sculpted. Looking back on that time 14 years ago, she wonders if that sudden move was the first hint of her husband’s Alzheimer’s disease. It took a decade for him to start forgetting his keys and stumbling on words. He passed away last year.
The Koopers’ experience is just one story out of millions: Every 66 seconds, someone in the United States is diagnosed with Alzheimer’s disease. Currently 5.5 million people in the country live with the condition, and there is still no known way to prevent or cure the disease. With baby boomers getting older, doctors are preparing for a huge wave of Alzheimer’s patients—and the nation will have to figure out how to pay for their care. Today, there are drugs that can slow the symptoms of Alzheimer’s, but they can’t yet stop it.
USC has committed itself to tackling Alzheimer’s, and more than 70 researchers, physicians and scientists at the university work to attack a problem considered a looming health and economic crisis.
The Root of the Problem
 Alzheimer’s disease has been a tricky illness to crack for several reasons, says Helena Chui, chair of the Keck School of Medicine of USC’s Department of Neurology. Alzheimer’s is a prototypic neurodegenerative disorder, which means it’s part of a class of disorders in which neurons in the brain die slowly, causing irreversible tissue shrinkage and damage. Other diseases in this category include Parkinson’s and ALS, also called Lou Gehrig’s disease.
Alzheimer’s disease has been a tricky illness to crack for several reasons, says Helena Chui, chair of the Keck School of Medicine of USC’s Department of Neurology. Alzheimer’s is a prototypic neurodegenerative disorder, which means it’s part of a class of disorders in which neurons in the brain die slowly, causing irreversible tissue shrinkage and damage. Other diseases in this category include Parkinson’s and ALS, also called Lou Gehrig’s disease.
Researchers haven’t learned how to slow or cure any of those disorders, Chui points out, and part of the reason is the complexity of the brain. In infectious diseases, physicians know the cause of a problem and can usually treat it. “If it’s like pneumonia or bacterial diseases, we have antibiotics,” Chui says, but in Alzheimer’s disease, “we still don’t know the culprit.”
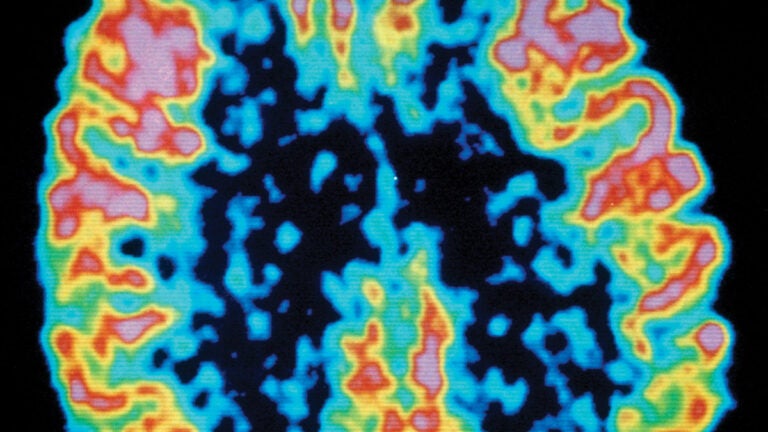
Alzheimer’s disease starts slowly, sometimes taking a decade or more before cognitive problems appear. Abnormal deposits of proteins called amyloid and tau build up throughout the brain, forming plaques and tangles. Then once-healthy neurons, or nerve cells, stop functioning, lose connections with other neurons, and die. The damage initially appears to take place in the hippocampus, which is the part of the brain essential in forming memories. As more neurons die, additional parts of the brain are affected.
For decades, scientists have looked to plaques and tangles to make a diagnosis, but it’s still an open question as to when they appear in the course of the disease. “Plaques and tangles could be on the direct causal pathway or could be a reaction to what is going on,” Chui says. Scientists have known that the accumulation of amyloid peptides in the brain drives Alzheimer’s disease, yet no effective anti-amyloid therapy exists for slowing down Alzheimer’s.
 Paul Aisen, a neuroscientist who leads the Keck School of Medicine’s Alzheimer’s Therapeutic Research Institute, points out that the disease, first described in 1906 by the physician Alois Alzheimer, was considered a rare disease of middle age for most of the 20th century.
Paul Aisen, a neuroscientist who leads the Keck School of Medicine’s Alzheimer’s Therapeutic Research Institute, points out that the disease, first described in 1906 by the physician Alois Alzheimer, was considered a rare disease of middle age for most of the 20th century.
“It was only in the 1970s that the field recognized that senile dementia—a common disease of the elderly—was the same as the one Dr. Alzheimer described,” Aisen says. “Now we know this isn’t a rare disorder; it’s the most common dementia of aging.”
Even though results of many clinical trials of potential drugs have disappointed researchers, Aisen is hopeful. “I think we’ve made tremendous progress,” he says. “I now believe that we are on the cusp of effective therapies for Alzheimer’s disease.”
One of the important lessons researchers have learned over the past three decades of tracking Alzheimer’s is that it doesn’t begin with the symptoms you’d commonly identify with the disease, such as memory loss. It used to be that Alzheimer’s disease couldn’t even be definitively diagnosed until after death—no scanning technique was sophisticated enough to see the plaques and tangles in a living person.
When a patient’s symptoms were bad enough to interfere with daily living, doctors would call it “probable” Alzheimer’s, Aisen says. But it turns out that this diagnosis was incorrect about 20 percent of the time, something doctors would only discover later during autopsies. “So we’d be testing drugs on people who didn’t have plaques and tangles,” he says. “That leads to difficulty in establishing drug benefits.”
Finding It Early
Researchers see great hope in reframing Alzheimer’s disease into stages and hunting for symptoms of very early stages of the disease, where they can make a huge impact.
When large clinical studies began to follow people for many years, the field started to crack some fundamental parts of the disease, Aisen says. “One of the things we began to understand is that the plaques and tangles actually start to appear in the brain about 15 to 20 years prior to the physical manifestation of dementia.”
Using PET scanning—a technology that detects radioactive tracers injected into the body—researchers can now detect the beginning of amyloid buildup in the brain. That’s a sign that seems to accurately determine who is going to develop Alzheimer’s.
Peering into brains early—before symptoms appear—could be a game-changer for the hunt for Alzheimer’s treatments. Right now, treatments are targeted at people who are in what Aisen calls the late stage of the disease, when it has already substantially damaged the brain. It’s like trying to slow down a freight train: “At some point, it becomes too late, especially if your intervention is targeting the wrong stage,” he says.
Aisen’s study shows that roughly a third of the population over 65 has amyloid plaques in their brains. USC has been following these patients for about 13 years, and during that time, 85 percent of the people who showed amyloid accumulations in the PET scan have developed symptomatic Alzheimer’s disease.
“We think it’ll be 100 percent of the patients who develop the disease by the time 20 years is up,” he says. “It is our opinion that if you have these brain changes, you are going to develop symptomatic Alzheimer’s disease if you live long enough.”
Staggering Numbers
The oncoming wave of Alzheimer’s patients is even bigger than researchers originally thought.
Right now, life expectancy is around 82. The longer people live, the more Alzheimer’s disease there will be.
 It’s one of the world’s biggest health problems, says Julie Zissimopoulos, associate professor at the USC Price School of Public Policy. In the journal Forum for Health Economics & Policy, Zissimopoulos and her colleagues modeled what the economic situation would be as baby boomers age and demographics shift. What they found was shocking: They estimatedthat the financial burden of Alzheimer’s disease in the United States will skyrocket from $307 billion annually to $1.5 trillion.
It’s one of the world’s biggest health problems, says Julie Zissimopoulos, associate professor at the USC Price School of Public Policy. In the journal Forum for Health Economics & Policy, Zissimopoulos and her colleagues modeled what the economic situation would be as baby boomers age and demographics shift. What they found was shocking: They estimatedthat the financial burden of Alzheimer’s disease in the United States will skyrocket from $307 billion annually to $1.5 trillion.
Not only will the number of people with Alzheimer’s triple between 2010 and 2050, the cost of taking care of each person is also expected to double from $71,000 in 2010 to $140,000 in 2050.
However, those numbers depict a scenario where treatments aren’t available. Zissimopolous says that there is another important takeaway: Small advances can make a big difference in slowing the growth of health care costs. “We don’t need to hit a home run,” she says. “Even delaying the onset of the disease by one year has enormous benefits for individuals and society.”
Possible prevention?
Since those treatments are still in the future, patients who are diagnosed today try to live as well as possible. When Eleanor Kooper was caring for her husband, she wanted to make sure that he had the best possible chance of living a healthy life. So she stocked up on organic food, arranged for a personal trainer and made sure that he had music, art and other stimulation in his life even when he lived in care facilities.
We’ve made tremendous progress. I now believe that we are on the cusp of effective therapies for Alzheimer’s disease.
Paul Aisen
There are many reasons to eat healthful food, reduce stress and work out. Chui says they might cut the risk of neurodegenerative diseases like Alzheimer’s. “Exercise and eating well may help reduce the rate of these harmful processes, but we haven’t proved it yet,” Chui says. “It’s also true that sleeping well is important, because amyloid clears more when sleeping.”
The biggest risk factor for developing Alzheimer’s is simply aging, because the plaques and tangles accumulate over time. In addition, blood vessels help clear the plaques from the brain, so keeping a healthy cardiovascular system is also important.
Genes are also a factor. One rare type of early-onset Alzheimer’s is caused by a mutation in one of three genes, and its symptoms begin at a young age, often when patients are in their 30s to 50s. John Ringman, a Keck School of Medicine professor of clinical neurology and researcher, studies families with this form of inherited Alzheimer’s disease. By using various kinds of scans and examining spinal fluid, he studies the changes that occur in the brains of people who have the mutation but don’t yet have symptoms. Understanding this early-onset type of disease may help develop better treatments or interventions to prevent the later-onset disease, he says.
 As is often the case with disease risk, genes and the environment seem to interact in Alzheimer’s. Ask Caleb Finch, gerontologist at the USC Leonard Davis School of Gerontology, who has spent decades studying the effects of aging in relation to air pollution, nutrition and more.
As is often the case with disease risk, genes and the environment seem to interact in Alzheimer’s. Ask Caleb Finch, gerontologist at the USC Leonard Davis School of Gerontology, who has spent decades studying the effects of aging in relation to air pollution, nutrition and more.
Finch and USC colleagues Jiu-Chiuan Chen, associate professor of preventive medicine, and Constantinos Sioutas, professor of civil and environmental engineering, developed the first evidence that the gene variant APOE4, a major risk factor for Alzheimer’s disease, also increases vulnerability to air pollution. The researchers studied detailed medical assessments of more than 3,600 women in their mid-60s to late 70s from the Women’s Health Initiative Memory Study. They found that older women nearly doubled their dementia risk if they lived in places with fine particulate exposure higher than the Environmental Protection Agency’s standard, and effects were stronger in women who carried the APOE4 variant. If the finding holds up in the general population, small particles in outdoor air could account for roughly 21 percent of dementia cases worldwide.
“Essentially what we are observing is that the inflammation caused by environmental pollution increases the processes leading to Alzheimer’s,” Finch explains.
This is the first time that researchers have shown an interaction between particulates and APOE4. “In other words, you need to know not only what genes a person is carrying, but also their environment,” Finch says.
Beyond the Barrier
 Berislav Zlokovic, director of USC’s Zilkha Neurogenetic Institute and its Center for Neurodegeneration and Regeneration, has been thinking about a different kind of environment: leaky vessels around the brain. Zlokovic studies the blood-brain barrier, a physical gatekeeper that keeps toxic substances and pathogens such as bacteria and viruses from reaching the brain.
Berislav Zlokovic, director of USC’s Zilkha Neurogenetic Institute and its Center for Neurodegeneration and Regeneration, has been thinking about a different kind of environment: leaky vessels around the brain. Zlokovic studies the blood-brain barrier, a physical gatekeeper that keeps toxic substances and pathogens such as bacteria and viruses from reaching the brain.
Zlokovic was the first scientist to propose that flaws in the blood-brain barrier and impaired blood flow drive neurodegeneration, which contributes to all kinds of neurological disorders from Parkinson’s to Alzheimer’s. The idea is that the brain doesn’t function alone in the system: It depends on healthy blood vessels. When the vessels work improperly due to age or other factors, the system starts to break down and the brain’s function can be compromised.
One reason so many Alzheimer’s treatment trials have failed, according to Zlokovic, is that they don’t take into account the whole vascular system. “You can have great treatments, but they won’t succeed in the brain environment if the vessels are not working properly to supply blood and oxygen and clear toxins,” he says. “If you don’t treat the whole system, you may have only a short-lasting effect or no effect at all on brain functions.”
USC has committed itself to tackling Alzheimer’s, and more than 70 researchers, physicians and scientists at the university work to attack a problem considered a looming health and economic crisis.
He estimates that up to 45 percent of all dementias worldwide are wholly or partly due to age-related small-vessel disease of the brain. His team plans to further study blood vessels in neurological diseases, including the role of pericytes, the sentinel cells stationed at exclusive doorways through the blood-brain barrier.
Zlokovic is working on addressing Alzheimer’s disease on many fronts, from studies in the living human brain to animal and stem cell models. One line of attack is testing to see if a neuroprotective enzyme developed by his team for stroke patients can stabilize the vascular system in mice and rats with Alzheimer’s. That would theoretically delay disease onset, stabilize blood vessels and slow the accumulation of plaques and tangles. “There are a lot of things happening, and I’m very pleased with that, because we have been proposing vascular contributions to Alzheimer’s for a number of years,” he says. “I think it’s a very good time for Alzheimer’s disease efforts.”
Another innovative approach may come in the form of a brain prosthesis with the potential to restore long-term memory for people who have dementia or are recovering from stroke. USC Viterbi School of Engineering’s Ted Berger, a professor of biomedical engineering, is working on a technology that could help those suffering from short-term memory loss retain new information that can be recalled again. The implantable device is designed to bypass a damaged hippocampal section of the brain and provide the next region with a correctly translated memory.
Imaging the Future
 For Arthur Toga, director of the USC Mark and Mary Stevens Neuroimaging and Informatics Institute, watching his mother pass away from Alzheimer’s disease humanized the work that he was already doing on brain imaging. “A lot of us in research focus on the biology or imaging, reducing it into data,” he says. “But the fact of the matter is that Alzheimer’s is a disease that affects [people’s] lives and their families. So for me, having a mom who died of the disease links the science to the personal story.”
For Arthur Toga, director of the USC Mark and Mary Stevens Neuroimaging and Informatics Institute, watching his mother pass away from Alzheimer’s disease humanized the work that he was already doing on brain imaging. “A lot of us in research focus on the biology or imaging, reducing it into data,” he says. “But the fact of the matter is that Alzheimer’s is a disease that affects [people’s] lives and their families. So for me, having a mom who died of the disease links the science to the personal story.”
It’s an energy he takes to his work. Toga and his colleagues are collecting brain scan images of people in the early stages of Alzheimer’s. The comprehensive sets of images include detailed descriptions of anatomy, the integrity of the blood-brain barrier, and images that describe brain function with patients performing tasks. “All of these collectively now provide a richer data set from which we can characterize where the disease process is,” Toga says. Together, this rich information can help researchers develop a biomarker signature that more fully describes how the brain functions in people with Alzheimer’s compared to those with normal, age-related problems.
ALZHEIMER’S DISEASE RESEARCH TIMELINE
[iframe src=”https://cdn.knightlab.com/libs/timeline3/latest/embed/index.html?source=1Skr9n_84JbDKolE1312AB1S0kiWVUwuyW0wcg53877s&font=Default&lang=en&initial_zoom=2&height=650″ class=”full” height=”650″ webkitallowfullscreen mozallowfullscreen allowfullscreen frameborder=’0′]
In addition, Toga and his team are developing huge databases of brain scans from around the world. The project has become an important way of examining vast amounts of data to identify patterns and trends that might not have been visible otherwise, Toga says.
For example, women were once thought to develop Alzheimer’s disease at 1.5 times the rate of men—an observation published in 1997. “Since we now have aggregates of vast amounts of data, we went back and looked at 58,000 subjects to make comparisons between men and women,” Toga says. “We found that men and women are largely equivalent except in a very narrow decade of life, ages 65-75.” That finding was revolutionary. Drug trials could have been designed better if scientists knew that men and women are equally likely to develop the disease.
The way to study Alzheimer’s is to study people: You have to participate. You have to be part of the solution. People must take ownership of this problem.
Arthur Toga
Toga suggests that in the future, it’s likely that researchers will find a biomarker that identifies patients earlier in the progression of the disease so they can have a treatment that slows the process, similar to how statins are prescribed to people with high cholesterol. Today, by the time that symptoms send someone with Alzheimer’s to see a doctor, Toga says, a lot of brain tissue has already been lost. Combining treatments with early biomarkers—based on complex scans—could start to address the disease early and potentially slow or stop it.
Alzheimer’s continues to be one of the most complex health challenges facing researchers, but one meaningful way that the public can help is to partner with researchers and sign up for studies, Toga points out. Investigators need patients to join in large numbers to advance the science. “The way to study Alzheimer’s is to study people: You have to participate. You have to be part of the solution,” he says. “People must take ownership of this problem.”
Helena Chui likens participating in a clinical trial to joining a team. “It’s altruistic in a way,” she says. “There might not be an immediate benefit, but every trial is informative and it’s so important for the next generation.”
Eleanor Kooper agrees. She enrolled her husband, a USC patient, in a new drug trial for 18 months. The trial was halted, but she encourages everyone to take part in clinical research. “I told Ron, if there is any chance that this will help you or help the kids, you’ve just got to do it,” she says.
Her husband was the third member of the family to have Alzheimer’s disease, and her thoughts are now with her children: If clinical trials today can help them 20 years from now, it’s worth it to participate. Ron Kooper also agreed to donate his brain to Alzheimer’s disease research after his death. It’s just another way that he was always helpful, kind and thinking of others, Eleanor Kooper says.
“For a long time, Alzheimer’s was like a dirty little secret,” she says. “Now people are talking about it, and they have to. We have to protect our future.”
Interested in research studies related to Alzheimer’s disease? Explore the Alzheimer’s Therapeutic Research Institute’s active studies list.