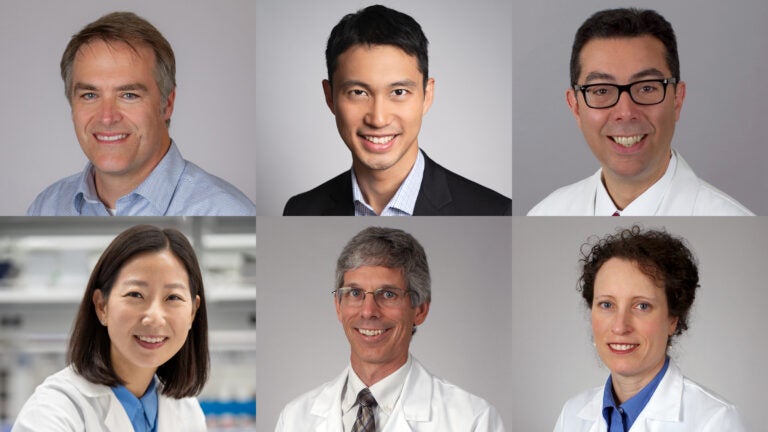
One group of NEMO Prize recipients consists of Brian E. Applegate, Wade Hsu and John S. Oghalai (top row, from left); the other group is Eun Ji Chung, Ken Hallows and Nuria Pastor-Soler. (Hsu Photo/Courtesy of Wade Hsu; Chung Photo/Chris Shinn; all other photos/Ricardo Carrasco III)
First NEMO Prizes fund research partnerships at the intersection of health and engineering
Awards were given to two USC research teams to fund collaborations between engineering and one or more of the university’s five health sciences schools.
USC’s Office of the Senior Vice President for Health Affairs has awarded the university’s inaugural NEMO Prizes to two teams of USC researchers across the University Park and Health Sciences campuses.
The NEMO Prize originates from a generous gift from Shelly and Ofer Nemirovsky. After Ofer Nemirovsky, a University of Pennsylvania business and engineering graduate, started the prize at his alma mater, the couple looked for an opportunity to do the same at USC, from which Shelly Nemirovsky graduated in 1985 and now serves on the Board of Trustees and as a member of the President’s Leadership Council.
“It’s really life-affirming for me to watch what can happen when the right minds get in the right room together,” Shelly Nemirovsky said. “The notion of putting the school of engineering and school of medicine together, and what they might accomplish — it’s just extraordinary.”
The winners of the highly selective $125,000 prizes — which will be presented annually to two teams for the next five years — proposed projects designed to bridge the gap between ideas and clinical breakthroughs in health and engineering collaborations. The prize aligns with President Carol Folt’s Transforming Health Sciences “moonshot,” which leverages USC’s research, medical training and clinical care to innovate and better serve patients and the community.
One of the winning projects, “RNA-BASED Nanoparticle Therapy for Polycystic Kidney Disease,” includes Keck School of Medicine of USC Professor Ken Hallows and Associate Professor Nuria Pastor-Soler, director and co-director, respectively, of the USC Polycystic Kidney Disease Clinic at Keck Medicine of USC, in collaboration with Associate Professor Eun Ji Chung, the Dr. Karl Jacob Jr. and Karl Jacob III Early-Career Chair at the USC Viterbi School of Engineering. The trio aims to perfect a therapy to target the root cause of polycystic kidney disease, before patients need dialysis or a kidney transplant.
The second group of prize winners includes electrical and computer engineering professor Wade Hsu and otolaryngology — head and neck surgery and biomedical engineering professors Brian E. Applegate and John S. Oghalai in a project titled “Through-Bone Optical Tomography of the Human Cochlea.” Prize funds will go toward developing a method for imaging the inner ear to address issues related to hearing loss and vertigo.
“These awards are an exciting reflection of the power of collaboration between engineering and health sciences, and how individual strengths are magnified when researchers from different schools combine their skills, expertise and dedication to scientific discovery,” said Steven D. Shapiro, USC’s senior vice president for health affairs. “Together, we are stronger as we continue our mission of delivering lifesaving medical care and research.”
Targeting the root cause of disease
Hallows describes polycystic kidney disease (PKD) as one of the most common, potentially lethal genetic diseases, cutting across all backgrounds. According to the research team, roughly half of patients with PKD will need kidney replacement therapy by the age of 50 to 60 years old.
The only FDA-approved therapy for PKD is a drug called tolvaptan, which isn’t well-tolerated in a large percentage of patients, Hallows said. Because the medication is taken orally, it can affect other organs in the body and cause issues such as frequent urination and liver dysfunction.
“There’s really a need for new therapies [for PKD] that are well-tolerated and target the root cause of the disease while correcting downstream signaling pathways that are dysregulated in the disease,” Hallows said. The team specified that almost all people with PKD have a mutation in one of two proteins called polycystins, which are encoded by the genes PKD1 and PKD2. These proteins are important for normal cellular function and growth control, as well as the polarity of cells that line the kidney, liver and other organs.
“The therapy that we won the NEMO Prize for is actually targeting those underlying mutations,” Hallows said. The team plans to address the genetic basis of the disease directly through mRNA delivered using nanoparticles, a method Hallows and Chung have collaborated on for the past seven years. While nanoparticles have been used as delivery systems in medicine for years — including with drugs to treat other diseases in other tissues — the team’s method is unique in that the delivered mRNA will go straight to the kidney to target the specific mutation found in the majority of PKD patients, ideally without side effects in other parts of the body, Chung said.
Chung, a nanoparticles engineer, first began developing nanoparticles designed to treat heart disease as a postdoctoral researcher at the University of Chicago. She noticed that the nanoparticles would go to the kidneys when the size and surface was tuned, which sparked an “aha” moment for the engineer.
“It was a coincidence that ultimately led to a lot of new innovation in my group,” said Chung, whose team became well-known for kidney nanomedicine after the discovery. “For the kidney, there’s just been a lack of innovation.”
When Chung made the move to USC, she reached out to Hallows, who shared his research interest in PKD that he was already working on with Pastor-Soler. The pair have been collaborating since then.
“The NEMO Prize has the potential to be transformational,” Pastor-Soler said. “The fact that they’re putting resources to support these types of collaborations is really encouraging and really timely.”
Using innovation to treat a growing health issue
The second winning USC team also views their NEMO Prize as an opportunity to use innovation to address common, hard-to-treat illnesses. According to the World Health Organization, by 2050 nearly 2.5 billion people will be living with some degree of hearing loss worldwide. At least 700 million will need some form of rehabilitation services. While there are many health issues that can lead to a diagnosis of hearing loss and vertigo — another issue involving the inner ear — Oghalai said there are few options for pinpointing a root cause. “MRIs and CT scans are all we have right now, and the resolution is too low to see any of the cells or tissues,” he said.
Applegate and Oghalai have worked toward addressing this issue for many years using a technique called optical coherence tomography (OCT) — commonly used by ophthalmologists to look at the inner part of the eye — to image the inner ears of both human and mouse subjects. While the technique has been very successful in mice, imaging human subjects has been challenging because our inner ear is blocked by a “thicker layer of bone,” Hsu said. This is an issue because bone scatters light, distorting imaging attempts of the inner ear. “The reason we send a telescope into space is so you don’t have the distortion of trying to look at a star through the atmosphere,” Oghalai said. He explained that the equivalent in a human would be sticking a tiny endoscope into the inner ear, which would be damaging.
Recently, however, Hsu’s group has begun developing a computational imaging method called scattering matrix tomography (SMT) that uses computer applications typically used in astronomy to improve the resolution and depth of imaging for the inner ear.
With their NEMO Prize, the three hope to join forces to use Hsu’s computational imaging method to overcome the limitations Applegate and Oghalai have experienced with the OCT technique.
“Nobody has been able to image the inner ear of humans with the resolution needed up to now,” Hsu said. “We hope to be the first to do that.”
The team is currently using preliminary technology from this approach to scan the outer ear of patients while continuing to do clinical trials on dead mice. This immediate goal is to move on to live mice and, once Hsu’s algorithms are perfected, live humans. Their long-term goal is to develop a hand-held, noninvasive SMT-OCT device for accurate imaging from the ear canal, Applegate said. The medical instrument would aid in diagnosis, creation of therapeutic interventions and the investigation of new therapies to treat and prevent hearing loss and vertigo.
“We just are so thankful for SVP Shapiro’s office for organizing this, and for the Nemirovsky family for donating the funds to support this prize,” Oghalai said. “We’re super excited to get this to work, and I think it’s going to help people.”
Partnership as a key to success
“We are thrilled that our faculty will receive NEMO Prize funding to pursue their research on the human cochlea and on polycystic kidney disease,” said Yannis C. Yortsos, dean of USC Viterbi. “Their partnership with their research collaborators from the Keck School of Medicine is key to the success of their projects. Such interdisciplinary collaborations not only form an essential element of the NEMO Prize but are necessary in today’s increasing convergence of the disciplines in health sciences and engineering.”
The NEMO Prize Steering Committee sought applicants who proposed exciting health-engineering collaborations that will be competitive for future follow-up funding from other sources and have the potential to improve health, health outcomes and health delivery down the road.
“Sometimes it gets a little siloed in academia; this [award] gives people the opportunity to share in a way where they’re not competing, but rather working together,” said Shelly Nemirovsky, whose brother and two out of three children also attended USC. The couple also gave a gift to create the Nemirovsky Residential College at USC Village in 2017 and funds the Shelly and Ofer Nemirovsky Provost’s Chair. “My hope is that researchers continue to talk across schools to find the great palliative ways to treat some of these horrible diseases out there. I think the possibilities are really limitless.”