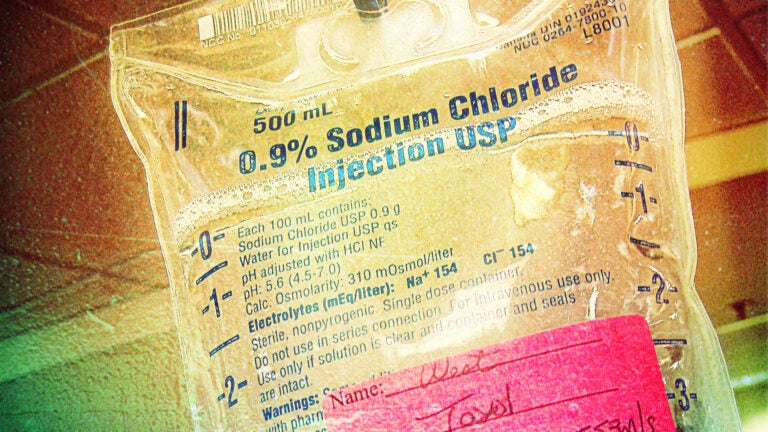
A USC researcher suggests that settings in which chemo is delivered should be controlled. (Photo illustration/Holly Wilder; Photo/Liz West)
Is there a kinder, gentler way to get chemo?
How changes in the environment might improve experiences during outpatient infusions
There’s no such thing as peaceful chemotherapy.
The anti-cancer drugs that attack the body’s dangerous cancer cells cannot discriminate from its healthy ones, causing immediate side effects such as nausea, fatigue, difficulty breathing and pain, not to mention long-term side effects including hair loss, organ damage and cognitive changes.
But what should be more purposefully controlled, according to USC researcher Leah Stein Duker, are the settings in which chemotherapy is delivered to patients.
“Multiple people in my life have been diagnosed with, and treated for, cancer,” said Duker, a research assistant professor at the USC Chan Division of Occupational Science and Occupational Therapy. “When I was sitting with them during chemotherapy infusions, I couldn’t help but observe how aspects of the environment — fluorescent lights, incessant noise, uncomfortable chairs and pervasive feelings of boredom and social isolation — all seemed to increase stress and anxiety.”
Those observations come naturally to Duker. For the past seven years, she has been on a National Institute of Dental and Craniofacial Research-funded research team studying the effects of sensory adaptations in the dental environment on physiological and behavioral stress in children with autism spectrum disorders during dental cleanings. The team’s promising findings suggest that environmental changes do indeed improve the dental care experience, and now Duker and her colleagues are investigating how and why this sensory adaptation intervention works.
What if we could make cancer treatment — chemotherapy infusions specifically — a little bit better?”
Leah Stein Duker
“What if we could also make cancer treatment — chemotherapy infusions specifically — a little bit better?” Duker asked. “What would make the infusion experience a kinder, gentler one?”
Raising awareness
September is National Childhood Cancer Awareness Month, a special initiative to highlight the types of cancer that largely affect children. About 10,380 children in the United States under the age of 15 will be diagnosed with cancer in 2016, according to statistics from the American Cancer Society. Because survival rates have dramatically increased during the last 20 years due to significant advances in diagnosis and treatment, more researchers are now focusing on the specific challenges faced during and following treatment.
While the types of “tailored environmental modifications” that Duker studies are in place at a handful of cancer treatment centers in Arizona and are used during rehabilitation at New York’s Memorial Sloan Kettering Cancer Center, their effects on pediatric populations during chemotherapy infusions have never been scientifically assessed — until now.
Thanks to funding from the National Institutes of Health’s National Center for Advancing Translational Sciences and a USC Zumberge Fund award that helps young faculty launch their research careers, Duker has begun a new research project to determine exactly what physical, sensory and social environmental factors are predictors of stress in children undergoing outpatient chemotherapy infusions and in their caregivers.
By conducting interviews and gathering physiological and behavioral data from children, their caregivers and health care providers at the Children’s Hospital Los Angeles Infusion Center, the Clinical and Translational Research Scholar hopes she can identify what environmental factors cause or alleviate stress during infusions. Duker will then use that data as a foundation to develop an intervention that modifies environmental factors during chemotherapy infusions in order to decrease children’s and caregiver’s behavioral, physiological and psychosocial stress.
By one day creating an intervention that offers customizable adaptations which reduce stress during outpatient infusions, Duker hopes her research can improve both the experience of chemotherapy and short- and long-term health outcomes.
“I truly believe that environmental adaptations have the potential to positively impact the experiences of people during any number of different stressful health care procedures,” Duker said. “Cancer is awful, but treatment doesn’t have to be.”



