One-third of all neighborhoods in the largest U.S. cities have been ‘pharmacy deserts’
Lack of geographical access to pharmacies has disproportionately affected Black and Latino city dwellers, a USC study finds, and may contribute to health disparities.
Black and Latino neighborhoods in the 30 most populous U.S. cities had fewer pharmacies than white or diverse neighborhoods in 2007-2015, USC research shows, suggesting that ‘pharmacy deserts’ — like so-called food deserts — may be an overlooked contributor to persistent racial and ethnic health disparities.
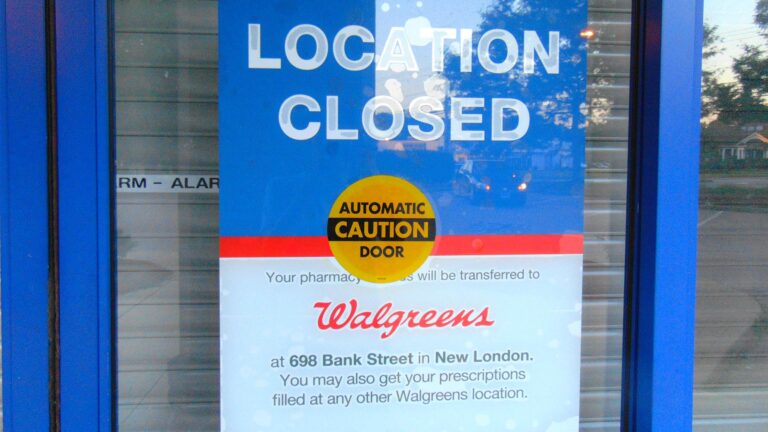
Pharmacies are increasingly vital points of care for essential health services. In addition to filling prescriptions to treat chronic health conditions, pharmacists dispense emergency doses of naloxone to reverse opioid overdoses, contraceptives to prevent unplanned pregnancy and COVID-19 testing and vaccinations.
But many neighborhoods in major cities such as Los Angeles, Chicago, Houston and Memphis lack convenient access to a pharmacy, according to research published today in the May issue of the journal Health Affairs.
“We focused on cities because of racial/ethnic residential segregation and the fact that more than 80% of the Black and Latino population in the U.S. live in cities,” said senior author Dima Mazen Qato, Hygeia Centennial Chair and associate professor of pharmacy at the USC School of Pharmacy and senior fellow at the USC Schaeffer Center for Health Policy & Economics.
“Our findings suggest that addressing disparities in geographic access to pharmacies — including pharmacy closures — is imperative to improving access to essential medications and other health care services in segregated minority neighborhoods,” added Qato, who directs the Program on Medicines and Public Health.
Traveling a mile … may be difficult for people who live in low-income neighborhoods and don’t drive.
Dima Mazen Qato
“One in three neighborhoods throughout these cities were pharmacy deserts, affecting nearly 15 million people,” said Jenny S. Guadamuz, the study’s first author and postdoctoral fellow at the USC Schaeffer Center and the Program on Medicines and Public Health at the USC School of Pharmacy. “However, limited access to pharmacies disproportionately impacts racial/ethnic minorities — 8.3 million Black and Latino residents of these cities live in deserts.”
Researchers focused on census tracts/neighborhoods in cities with populations of 500,000 or more. Census tracts, smaller than ZIP code areas, generally have a population size between 1,200 and 8,000 people. Data from the U.S. Census Bureau’s American Community Survey established neighborhood characteristics including total population, percentage of the population by race/ethnicity, low-income status and vehicle ownership. Pharmacy locations and types of pharmacies came from the National Council for Prescription Drug Programs.
Researchers overlaid census tract maps with pharmacy locations. Neighborhoods where the average distance to the nearest pharmacy was 1.0 mile or more were classified as pharmacy deserts. In neighborhoods that were low income and had at least 100 households with no vehicle, the qualifying distance dropped to 0.5 miles or more to account for transportation barriers.
“Traveling a mile to get your prescription medications may be convenient for people that own a car. Traveling a mile, or even half a mile, may be difficult for people who live in low-income neighborhoods and don’t drive, particularly older adults who rely on walking or public transportation,” Qato said.
Disparities in pharmacy deserts affect many American cities, including Los Angeles
Prevalence of pharmacy deserts varied widely across cities. In New York and Philadelphia, for example, fewer than 10% of neighborhoods met the definition of pharmacy deserts. On the other hand, more than 60% of neighborhoods in Indianapolis, San Antonio and Charlotte were pharmacy deserts.
In all cities, segregated Black or Latino neighborhoods, or both, were more likely to be pharmacy deserts than white or diverse neighborhoods. These disparities were most pronounced in Los Angeles, Chicago, Albuquerque, Dallas, Memphis, Boston, Milwaukee, Baltimore and Philadelphia.
“We observed stark disparities in Los Angeles, where one-third of all Black and Latino neighborhoods were pharmacy deserts, particularly neighborhoods in South Central L.A., including Florence, Broadway-Manchester and Watts,” Guadamuz said.
Policymakers need to make sure that stores serving Black and Latino areas are not excluded from pharmacy networks.
Jenny S. Guadamuz
Among all the cities examined, the most pronounced disparities were in Chicago, where 1% of white neighborhoods were pharmacy deserts in comparison to 33% of Black neighborhoods in the South Side neighborhoods of Chatham, West Pullman and Greater Grand Crossing, Guadamuz added.
The researchers said policies could help address the situation. For example, federal, state and local governments could deploy targeted grants and tax benefits to encourage pharmacies to locate in pharmacy deserts. Other incentives could motivate pharmacies to offer services such as home delivery to improve access.
“Increasing Medicaid and Medicare pharmacy reimbursement rates for prescription medications might encourage pharmacies to open in areas of need,” Guadamuz said. “To ensure existing pharmacies don’t close, policymakers need to make sure that stores serving Black and Latino areas are not excluded from pharmacy networks.”
In addition to Qato and Guadamuz, study authors include Jocelyn R. Wilder of the University of Illinois at Chicago; Morgane C. Mouslim of the University of Baltimore; Shannon N. Zenk of the National Institute of Nursing Research; and G. Caleb Alexander of the Johns Hopkins Bloomberg School of Public Health.
Funding for this study was provided by the National Institute on Aging (Qato, Grant No. R21AG049283) and the Robert Wood Johnson Foundation (Qato, Guadamuz and Zenk).



