Elyn Saks recently co-developed a care navigation phone service called Mental Health GPS, which helps connect callers with appropriate mental health care. (Photo/Courtesy of Mikel Healey)
Q&A with Elyn Saks: When your mind is your best friend and worst enemy
Elyn Saks is a renowned legal scholar and a skilled educator. She’s also a fierce advocate for mental health who evaded a dire prognosis after being diagnosed with schizophrenia at age 28.
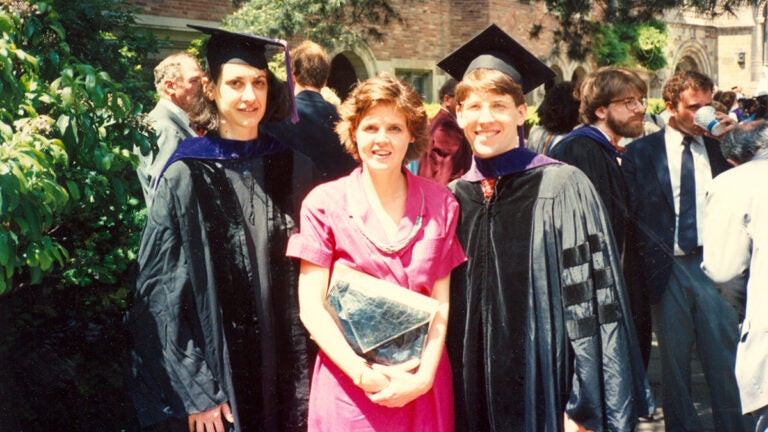
Elyn Saks is a renowned expert in mental health policy and law whose list of accomplishments is as long as it is impressive. She graduated from Yale Law School; directs the Saks Institute for Mental Health Law, Policy, and Ethics at the USC Gould School of Law; and is the recipient of numerous honors, including the prestigious John D. and Catherine T. MacArthur Foundation Fellowship (the so-called “Genius Grant”).
Saks also lives with chronic schizophrenia — a diagnosis she made public with her 2007 memoir, The Center Cannot Hold: My Journey Through Madness.
USC News sat down with Saks, who recently co-developed a peer-based care navigation service called Mental Health GPS and published findings from the yearlong pilot program, to discuss how her lived experience with mental health has informed her lifelong work advocating for systemic change and patients’ rights.
What inspired you to share your experiences with mental health?
Saks: I wanted to write a corrective story about the many faces of schizophrenia and mental illness. I was originally advised to write my memoir under a pseudonym, but I felt that would send the wrong message. I stayed true to that goal and wrote the memoir to give hope to those who suffer from schizophrenia and understanding to those who don’t.
Once, after publishing my memoir, I was scheduled to appear on a TV news show to discuss my experiences with mental health. But it was canceled at the last minute. I was told that I wasn’t “representative enough” of people with mental illness. But I believe that it is important to show the full range of experiences, including those who are doing well, and that remains a big part of my advocacy today.
What are some of the ways in which mental health disparities manifest in the legal system, and how can the system better support people with mental illness?
Saks: Within the U.S. legal system, disparities are often not brought to light. There are a lot of misconceptions about mental health and the law. For example, the insanity defense is often misunderstood, and people assume that individuals pleading insanity are getting off easy. But people put in forensic psychiatric institutes often spend as much time there as they would have if they’d been sentenced.
There are also issues around civil commitment, specifically who is being committed. There are significant racial/ethnic and gender-based disparities in civil commitment. It used to be the case that women were very easily committed because their husbands claimed they were not being a good wife or accused them of being promiscuous.
We run into similar issues with homelessness and mental illness. I often wonder why someone with a mental illness who is unable to provide for themselves can be involuntarily hospitalized, but someone with the same inability to provide for themselves who does not have a mental illness is not committed. And I can think of two reasons: One, if you have a mental illness, we can at least have the hope that if we get you treated, you’ll improve, stay out of the streets and find housing. Two, if you have a mental illness, you may have less capacity to make decisions.
What are you working on now?
Saks: I recently co-developed a peer-based care navigation phone service called Mental Health GPS, which helps connect callers with appropriate mental health care and avert crisis. I am a founding member on the board of INclude — the Mental Health Initiative, the nonprofit that operates Mental Health GPS. Results from the yearlong pilot recently published in the New England Journal of Medicine Catalyst: Innovations in Care Delivery and emphasize the importance of peer support. Peers know better than anyone else what it’s like to have these struggles. And they also are less likely to feel stigmatized interacting with each other.
Right now, we are studying who actually uses the information they are given to get care. In the future, I would also love to study the downstream effects of the program, including more independent living, more independent working and a better relational life.
I’m also doing empirical work around supported decision-making and psychiatric advance directives. That’s where you say, if I get sick, here’s where I want to go, these are the meds that work for me and the ones that I don’t want. Here is who I want to be told. It allows people to be the architects of their own lives. As someone who has had choice taken away, I can attest to its importance.